Shingles and the Eye
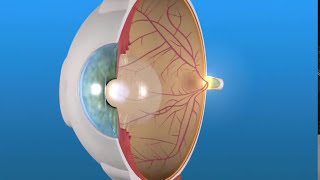
Before the varicella vaccine, almost all children contracted chickenpox. The virus then would lay dormant for 50, 60, or 70 years and then often flare up. The "flare up" of the chickenpox virus is what we call shingles. It is a localized resurgence of the virus in nerves of the body corresponding to a specific area called a dermatome. This is an area on the skin that could be on the torso, the face or the arms and legs. About 20% of the cases involve the upper eyelid and forehead and could possibly involve the eye. In my clinic, about half of those cases involve the actual eye and not just the eyelid. This condition can cause inflammation resulting in iritis, conjunctivitis, and keratitis (inflammation of the cornea). These problems need to be treated immediately in order to preserve vision and have the best outcome. Most patients need to be treated with valtrex, acyclovir, or famvir during the acute episode to decrease the risk of post-herpetic neuralgia and more serious side effects. Post-herpetic neuralgia is a condition of pain after the virus resolves. It results from nerve damage, and can often be severe. I will often treat this condition with medications including lyrica, neurontin, lidocaine patches, and amitriptyline. This is often the most significant long term problem that results from the shingles. The virus is usually killed by the body and combination of medication that goes against the virus; however, long term complications often ensue. Besides chronic pain, the dead virus usually lingers, and the body will cause inflammation over the long term in many of those cases. It is the chronic inflammation that can often result in the most damage and vision loss in herpes zoster of the eye. The patient will often need long term steroid drop treatment in order to maintain vision and comfort. It is not uncommon for a patient to feel and see better, but then slowly lose these gains as the inflammation smolders over several months. I will typically see a patient every week or so until the inflammation resolves and then see a patient every month or two until I am sure there is not going to be a repeat flare up. A lot of my patients will ask me about the getting the shingles vaccine. I believe that if you have not had shingles it is good to get the vaccine per the CDC recommendations. However, if you have had shingles in the eye, I would recommend possibly not proceeding with the shingles vaccine. There is some evidence that it could cause a flare up in the auto-immune disease; several case reports have mentioned this and there is a physiologic rationale for a flare. If you have chronic shingles in the eye, or a new episode, please contact our office at 512-686-1224 to see Dr. Aaker who is a cornea specialist.